Knee Osteoarthritis: Debunking Myths and Exploring Conservative Care
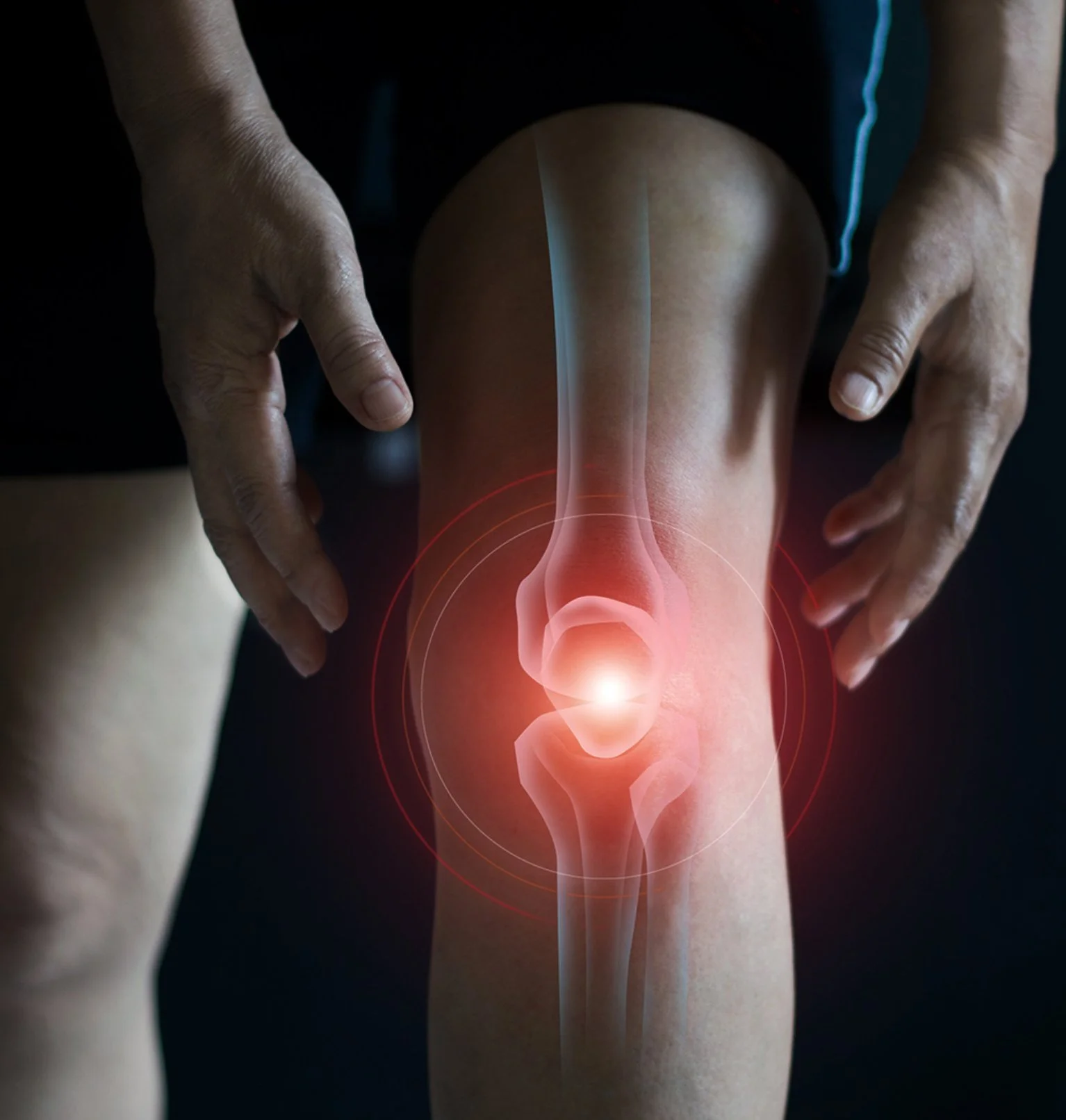
Knee osteoarthritis (OA) is one of the most common sources of joint pain in adults, yet it’s also one of the most misunderstood. For many patients, the term "arthritis" conjures up images of worn-out joints, irreversible damage, and an inevitable march toward joint replacement. But the reality is far more hopeful—especially when myths are cleared up and the right care is provided.
Myth #1: “It’s Bone on Bone”
One of the most alarming phrases patients hear is that their knee is “bone on bone.” While this term is often used to describe significant cartilage thinning, it’s rarely accurate. Most people still have some cartilage left, even in advanced OA. More importantly, the degree of arthritis seen on imaging does not always correlate with pain.
A landmark study by Bedson & Croft (2008) in BMJ found poor correlation between radiographic severity and reported knee pain. Many individuals with severe arthritis on X-ray have little to no pain, while others with minimal changes experience substantial discomfort. Pain is multifactorial—it’s not just about joint wear, but also inflammation, neuromuscular control, and central sensitization.
Myth #2: “If You Have Arthritis, You’re Doomed to a Knee Replacement”
Knee replacements can offer relief for some, but they are not the only option—and they should not be the first. A growing body of evidence supports exercise therapy, manual treatment, and weight management as first-line treatments for knee OA.
The 2019 Osteoarthritis Research Society International (OARSI) guidelines strongly recommend non-surgical interventions such as therapeutic exercise, education, and manual therapy before considering surgery. The American Academy of Orthopaedic Surgeons (AAOS) also advises delaying surgery in favor of conservative care whenever possible.
How Do You Know If OA Is the Cause of Your Knee Pain?
While X-rays can show joint space narrowing, osteophytes, and sclerosis, they don’t tell the whole story. A diagnosis of knee OA is best made clinically, based on signs like:
- Pain with weight-bearing activities
- Morning stiffness lasting less than 30 minutes
- Joint line tenderness
- Grinding or crepitus with movement
The clinical criteria developed by Altman et al. (1986) are still widely used, showing that a good physical exam can be just as valuable as imaging.
What Can Manual Therapy Do?
As chiropractors and manual therapists, we offer a range of treatments to manage knee OA without surgery or medication:
- Joint mobilizations to improve range of motion and reduce stiffness
- Soft tissue therapy (e.g., Active Release, IASTM) to reduce muscle tension
- Dry needling (when appropriate) to reduce pain and guarding
- Neuromuscular re-education to restore proper movement patterns
- Strength training for the quads, glutes, and hamstrings to stabilize the knee
- Education and lifestyle modification to promote long-term success
A 2013 study by Deyle et al. in Physical Therapy showed that manual therapy combined with exercise outperformed home exercise alone, with benefits lasting up to one year. And strengthening the quadriceps alone has been shown to reduce pain and improve function (Arthritis Care & Research, 2013).
We also assess the entire kinetic chain. Limitations in hip or ankle mobility can shift stress to the knee. Treating the knee in isolation rarely delivers long-term relief.
The Bottom Line
Knee osteoarthritis doesn’t have to mean giving up the activities you love. Imaging findings like “bone on bone” can sound dramatic, but they don’t dictate your future. With individualized care—focused on movement, strength, and manual therapy—most people can avoid surgery and regain control of their health.
At MVMT STL, we believe in empowering patients with real strategies that work—not fear-based narratives or outdated thinking. If you’ve been told that surgery is your only option, let’s explore a better one.